This piece is part of our Empowered Birth series, highlighting ways Black women can have birth experiences that leave them and their families feeling safe and respected. Click here for more stories.
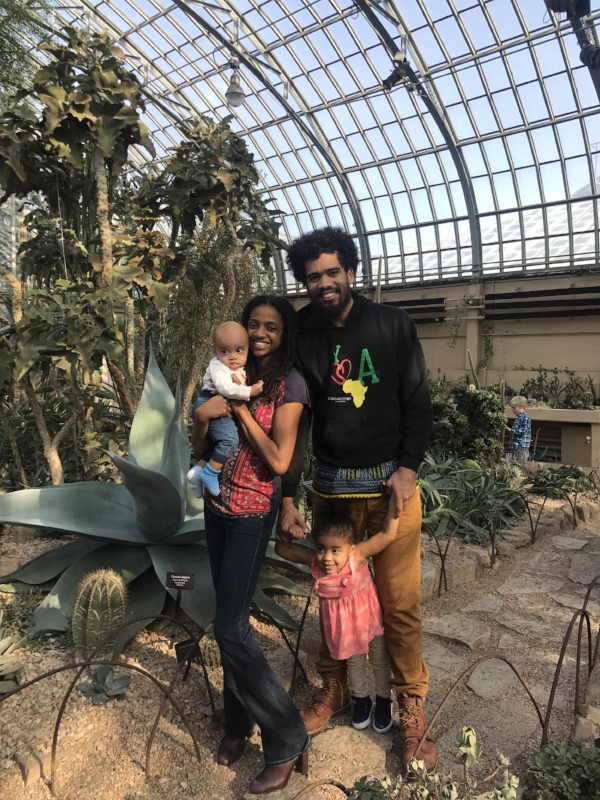
Tayo Mbande, 24, is a Chicago-based mom of two (her daughter, Yahya-Ayan is 2.5 years old, and her son Kamalu-Ime is 6 months). She’s the co-founder (alongside her mom!) of a birth and postpartum company called Chicago Birthworks Collective.
Tayo and her then-boyfriend found out she was pregnant with their daughter during her senior year at Howard University. (Now her husband, Aremu Mbande is the director of the African American Male Resource Center at Chicago State University.)
“I was like, My life is over,” Tayo says now. “Four years of being excellent and then I got pregnant.”
Despite her initial misgivings, Tayo was positive she wanted to become a mother. And she had a very set idea of what her pregnancy and delivery would look like: no drugs, no interventions.
“We are very, very proudly granola Black parents. Our kids are 100% vegan, breastfed, not vaccinated,” she says.
But when Tayo ultimately decided to be induced, it didn’t make her feel any less empowered.
“My birth with my daughter allowed me to have that freedom to say, ‘You’re still the boss even if you take this medicine that is not made out of hemp seed and organic cotton,’” she says.
Tayo’s first pregnancy set the stage for a fierceness and confidence that informed the choices she made when she was pregnant with her son almost two years later. She tells her empowered birth stories below.
Editor’s Note: The information contained here does not constitute medical advice. This is a retelling of one woman’s experience and beliefs, and is not a substitute for professional advice or reflects the beliefs of mater mea.
My husband and I were in a big transition: He was still in grad school and I had just graduated. I decided to move to Indiana, where my mom was living. I was 30 weeks pregnant.
I had to find a new doctor. I wanted a home birth, but I knew that trying to pay for and organize one was going to be impossible at 30 weeks.
The next best option was finding a midwife. I went to an office and got paired up with an OB. I told her what I wanted my delivery experience to be like. I wanted to be able to move, to push when I was ready. I wanted to be able to bend over or be on my hands and knees. I wanted to be able to eat. I didn’t want any medication—I didn’t want an epidural or any other types of intervention.
“I have to be honest with you,” she told me. “I would encourage you to find another doctor.”
When I met my midwife, I told her all the things I wanted, and she said, “As long as you’re safe and your baby’s safe, I’m not going to set restrictions on what you can and can not do.”
I was like, “I love you!”
A Change Of Plans
On my due date—August 19, 2015—I was 0% dilated. I was kind of discouraged, but I said, “We’ll wait. My body is preparing, and I just might need a little more time to prep.”
My midwife gave me a check-up ultrasound. When she measured the baby, my daughter was measuring at 9+ lbs.
She said, “I don’t advise you to wait two weeks if you’re carrying a 9-lb baby. You would be extremely exhausted trying to push out a potentially 11-lb baby. There’s the risk of having a C-section… Why don’t we start with an induction?”
“You’re not going to induce me,” I said. “I want to wait.”
She said, “It’s just not a good idea. Do a little bit of research, see which induction methods people are using, and see which one fits you.”
I didn’t consider that I could regulate my own induction. I thought Pitocin, epidurals—just drugs, drugs, drugs. So I looked into it, and decided I wanted the least invasive option. We chose Cervidil, but I said after that, I wanted to go through labor on my own.
I got my family’s blessing, too. They had heard me rant about not wanting any kind of intervention and here I was about to elect to have one. I kind of felt embarrassed.
But I said, “I don’t want to push out an 11-lb baby! As natural as I want this thing to go, I don’t want to do that.” And my family said, “Hey, this is your choice.”
I let my midwife know. She wanted to induce me the very next day. When I got to the hospital, my midwife had already given the nursing staff very clear instructions to let me do my own thing before she got there.
My midwife gave me four hours so we could have that one last chance before we started the induction. Guess who didn’t go into labor? Me! (Laughs)
So I said, “Let’s do it.”

I went in at 11 a.m., and at 4:00 is when I got the drug. Do you know within 10 minutes, my contractions were like, “Wassup? We in here!”
My entire labor was 12 hours from start to finish. I was extremely active in my labor and moved things along. I bounced on the ball. I had clary sage on my ankles, which reminds your muscles to relax when they’re supposed to so that your contractions work and your labor is shorter.
I had my grandma tucked away in a corner, my dad and my husband were coming in and out. My mom was like my acting doula—she was by my side the entire time. My mom put me in the shower. She washed and styled my locs—that really helped me focus on something else besides the pain. My mom has been my hairstylist my entire life so that was particularly special for me.
There were times I was in the bathtub just thinking that I was dying. My grandma would come in there and she would sit next to me in the tub, pour some water on my belly. Her and my mom would swap. It was really incredible having all that maternal energy in there. They were like, “You got this.”
There are some medical practices that can aid you if you allow them to work within your own framework.
But then, about seven hours in, I was at about 4 cm. I had worked my way up to 4 cm, I earned those 4 cm.
A nurse came in and said, “OK, you’re getting a new nurse. I want to tell you you’re doing a good job, but I would recommend taking Stadol. In exchange for not getting an epidural, just take this drug to get some rest so you can ride those waves from the Pitocin.”
I had no intention of taking Pitocin. But apparently she told the next nurse that I WANTED it.
So the new nurse comes in and I told her I didn’t want to take Stadol. This woman—this little redheaded white woman—went coo-coo crazy on me.
“Look,” she said. “I just delivered a baby in a car in the parking lot. What you’re going to do is get out of that tub. I already ordered the drugs, and you call me when you’re in that bed and ready for these drugs!”
I was like “Who you talking to?!”
I’m really dead at this point. I’m looking at my husband, I’m looking at my mom, and they’re like, “What do you want to do? This is your call. If you take these drugs, you are not any less powerful. You didn’t do anything wrong. You are taking these drugs because this is what you want for your body and for your birth experience.”
I cried. But I took them drugs so fast!
She gave me the Stadol and said, “You let me know when it kicks in.”
I said, “Well, how long does it usually…” and I passed out.
‘That’s What I Want’
Stadol makes you super drowsy, but it doesn’t take away the pain.
I’m like, Ahhhh! [Pauses] Ahhhh! [Pauses] It was horrible!
Did I sleep? No! But my muscles relaxed, so I went from 4 cm to complete in three hours.
My midwife took an hour to get there. She didn’t think I was going to be ready so fast, so she had gone home. She comes in and I’m like “Where were you?! I’m ready to push!”
She really helped me center myself. She said, “I know you’re in a lot of pain, but remember what you said you wanted. Do you want to move? Do you want to change positions?”
I’m like, “Yes! Yes! That’s what I want.”
I got up. I pushed for 45 minutes. She was crowning, but I could not get her out. It’s because she got a big-ass head. My husband’s head is enormous, and I should’ve known.
They had to give me an episiotomy, which my midwife and I had talked about as a possibility, so it didn’t come as a surprise.
The OB, at that point, was there because my midwife noticed that I was struggling. They gave each other the I’m about to cut her look. My midwife caught me catching the look and gave me the You know I’m going to cut you look, and I gave her the Please, hurry up and do it look.
She did, and I gave the biggest pushes I could ever imagine, and she popped out. And it was great.

My birthing team knew from the beginning that I didn’t want my daughter to be vaccinated, I didn’t want the antibiotics in her eyes, no vitamin K, nothing. That was really exhausting for me to have to remind the birthing staff after I had just given birth, but I did. I woke myself up, because I knew they had it on deck.
I told them, “As soon as I push that baby out, you need to put this baby directly on my chest and don’t touch her. Don’t touch her, don’t touch me.”
My baby and I were together for three hours. She never left my chest. They didn’t even clean her. And that was really important for me because once I decided to be induced and to take that medication, I was starting to think I had failed. But when I made that decision to say “OK, we don’t want any of these drugs for our child,” I was reminded I make these decisions.
I didn’t give myself room in the beginning to say “Hey, there are some medical practices that can aid you if you allow them to work within your own framework.” But I used those practices, those drugs, those procedures in my own plan and said, “I’m going to use this to achieve the outcome that I want. I’m not allowing anyone to force me to use these to achieve an outcome that they want.”
‘This Is My Body’
When I was pregnant with my son, I had a preterm labor scare at 29 weeks.
The doctor came in. “I’m going to check you before sending you home.”
Apparently my son was head down at zero station and she could touch his head.
“You’re going into labor,” she said. “Your contractions are 10 minutes apart.”
They gave me hella drugs to try and stop the contractions. I felt so bad, but I said, “I would rather take all this stuff and detox my body, then to have my baby come out way too early.”
I was at the hospital for 10 days because they could not stop my contractions. Those 10 days turned me into the beast that I am today. I told my doctors off every moment I could: “I do not want that. Give me this pill instead of this. No, I need to see the results from this ultrasound right now.” I sent my husband all around the hospital for answers.
At day 10, I told my doctor, “I am going to sign an AMA [against medication advice] if you don’t let me go.”
So I left. They wanted to put me on a very strict bed rest, but I did everything that I wanted. They sent me home with some medication that didn’t stop the contractions and had awful side effects. So I stopped taking them.
I made all of these decisions for myself. But what was hard about this pregnancy was that my husband had different feelings about what I should do.
He said, “I am not completely comfortable with these decisions that you’re making.”
I said, “I respect that, but you have to respect that I am the partner in this relationship that gets to carry our children, and this is my body.”

Every day I put my feet down on the floor, his body would just cringe. I was hella scared! I was afraid that all of this pride and energy I felt was going to backfire on me, and that something was going to go wrong with my baby because I said I didn’t want to take these meds, I didn’t want to lay in the bed.
But what helped me get over that fear was that I did a lot more research. I found out that I was having prodromal labor, which I had never heard of and none of my providers had even mentioned.
I reached out to everyone I knew—anyone who had any type of challenging labor, friends who are OBs… I did a lot of reading, and that gave me a little bit of peace when I thought I was going overboard.
When it was close to my due date, I was in a lot of pain because I was having contractions 10 minutes apart, every day, all day. And I chose to be induced again.
No one wanted me to get induced. They were like, “You waited so long, just wait a couple more days!”
I said, “No. I’m uncomfortable, and this is what I want for my body and my birth experience.”
After going through my son’s birth, I realize that I learned how to advocate for myself while I’m in pain and how to be flexible. If you have already determined “I do or don’t want this in my birth,” when you have to make an opposing decision, you can still make an empowered choice, based on the options in front of you.


















